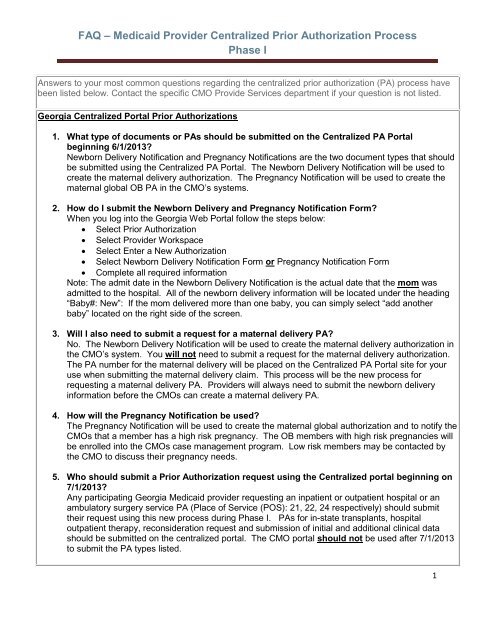
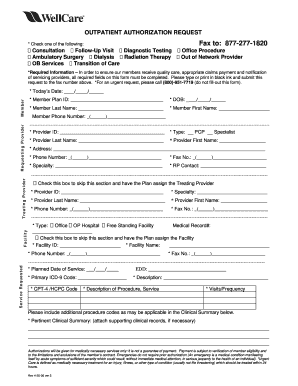
Georgia Wellcare Prior Authorization Form
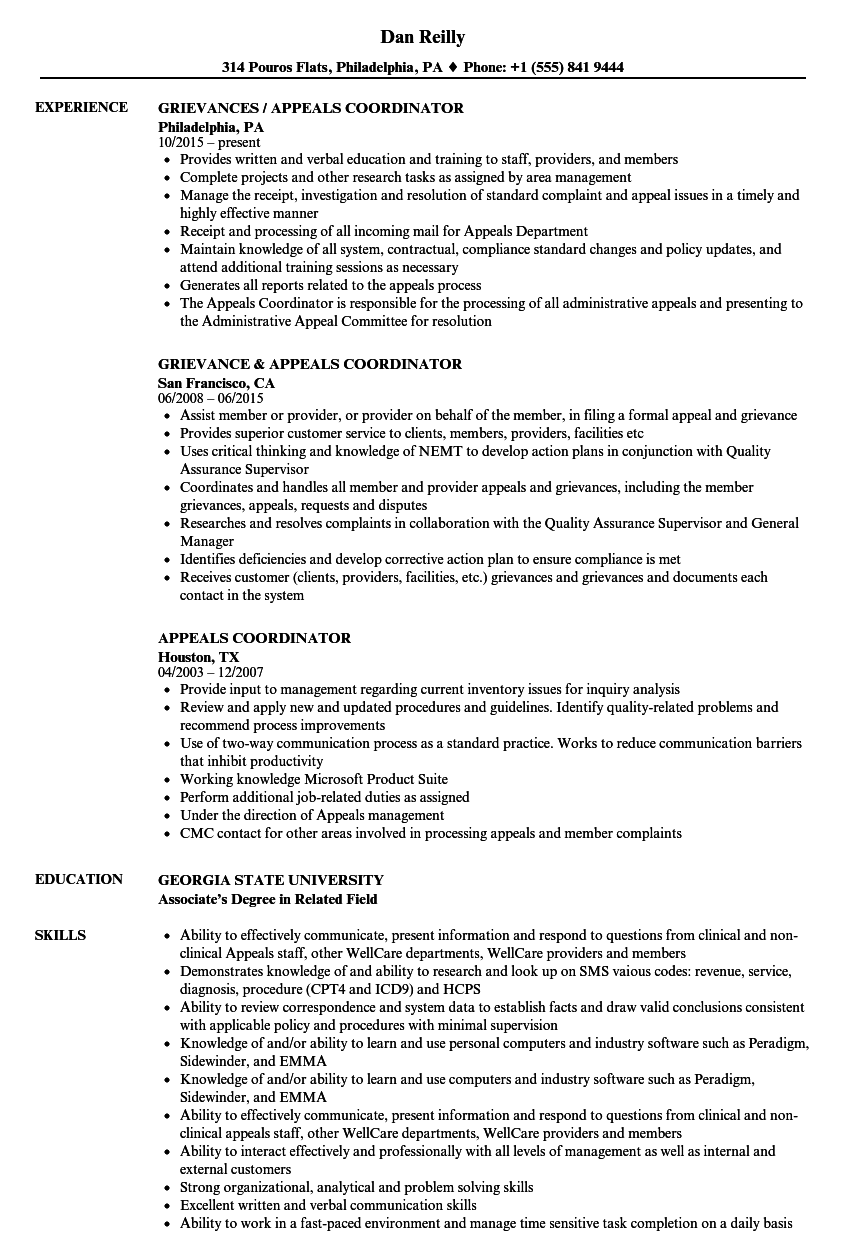
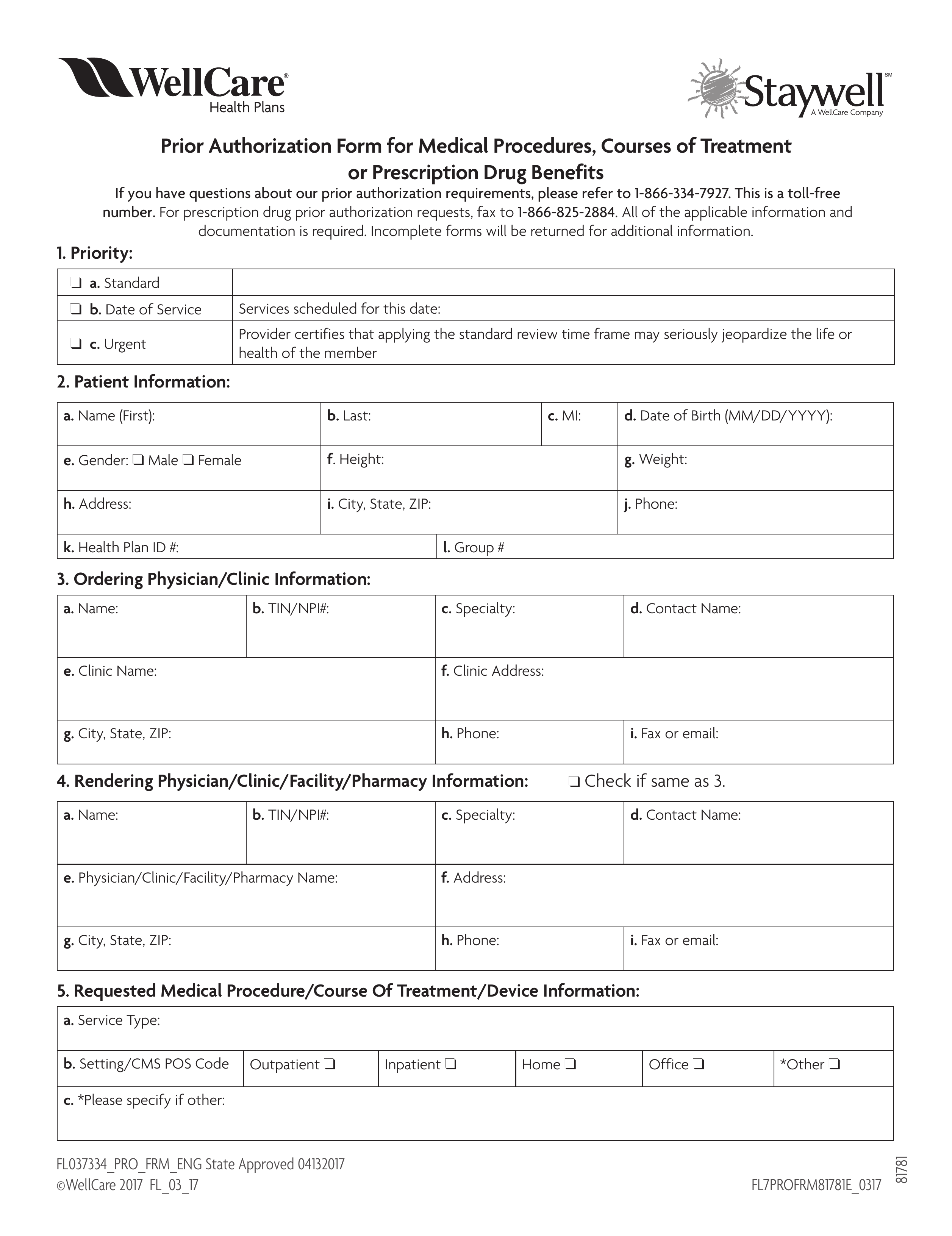
An individuals policy might not cover certain drugs procedures or treatments and a wellcare prior authorization form allows them or the prescribing physician to make a request for insurance coverage of the prescription in question.
Georgia wellcare prior authorization form. Coverage determination request form georgia. Prior authorization pa request process guide updated 13020. Trappe sandra m created date.
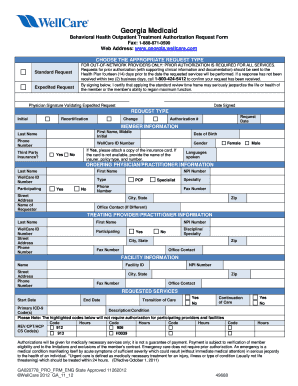
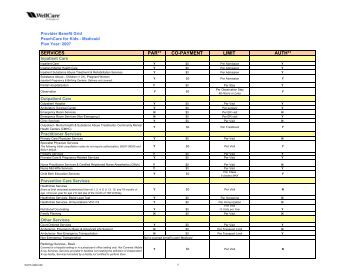
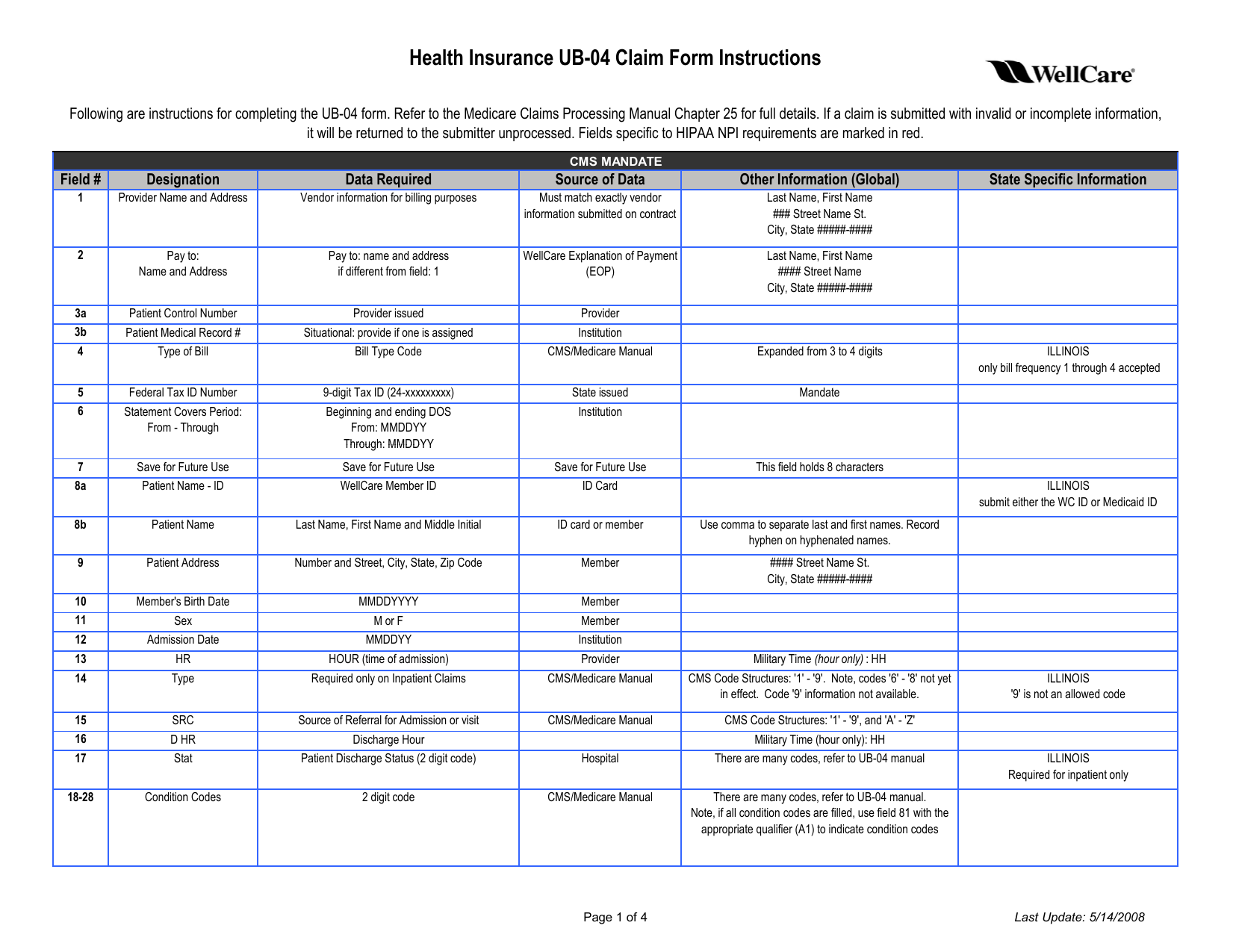
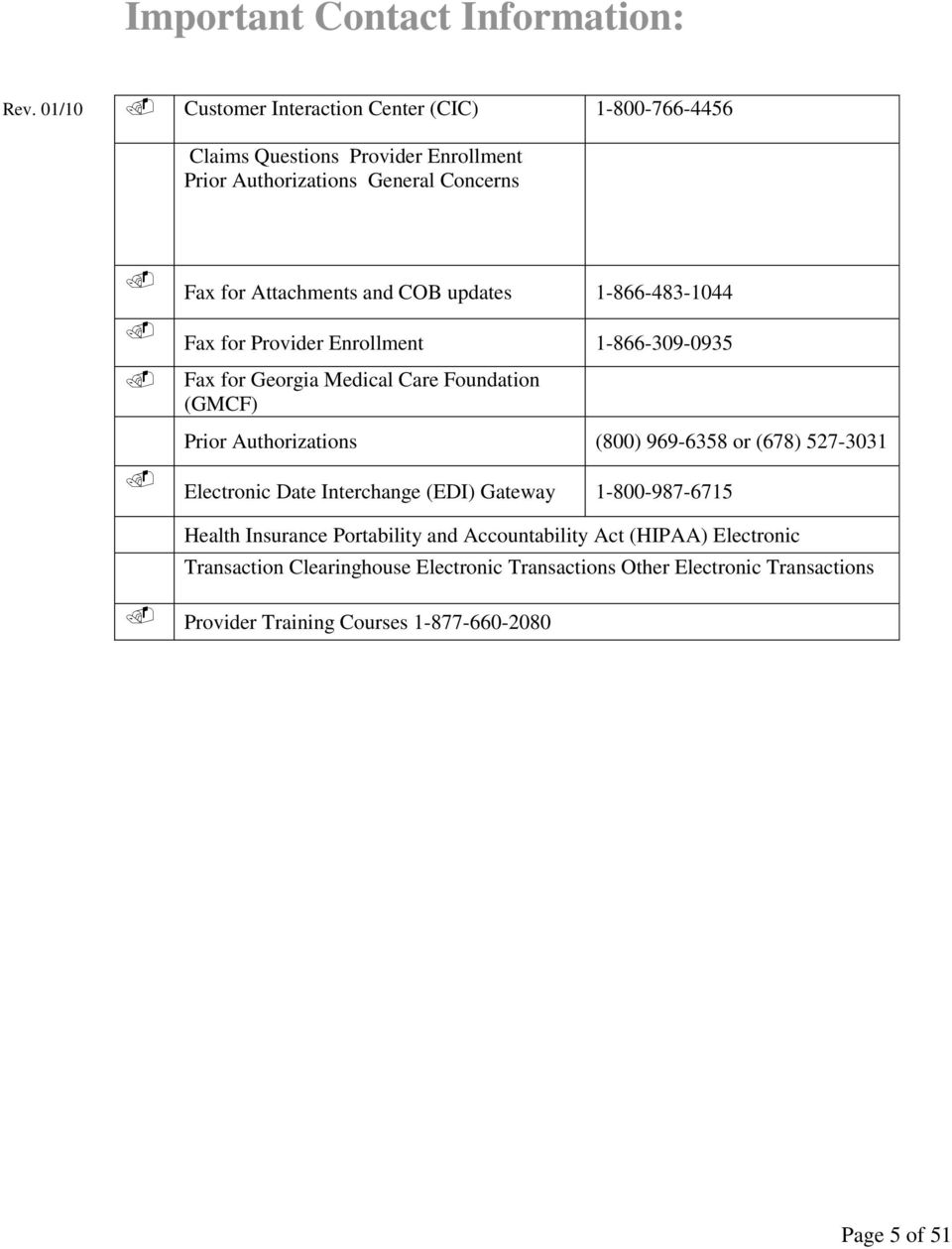
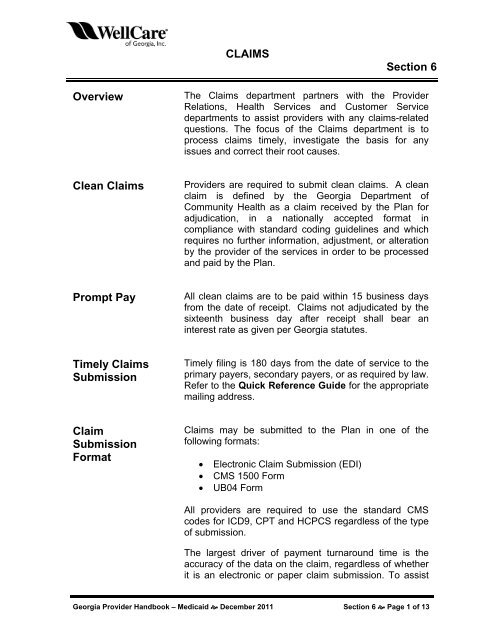
You should always use our websites authorization page to determine whether a procedure code requires prior authorization and always check eligibility and confirm benefits before rendering behavioral health services to members. Authorizations are valid for the time noted on each authorization response. Failure to obtain the necessary prior authorization from wellcare could result in a denied claim.
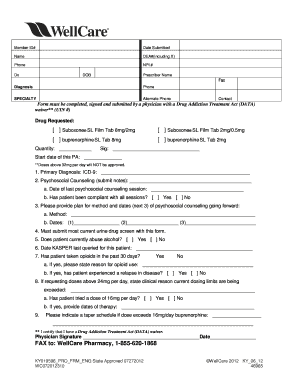
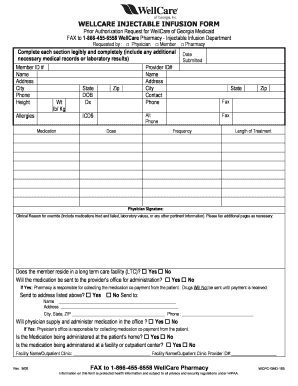
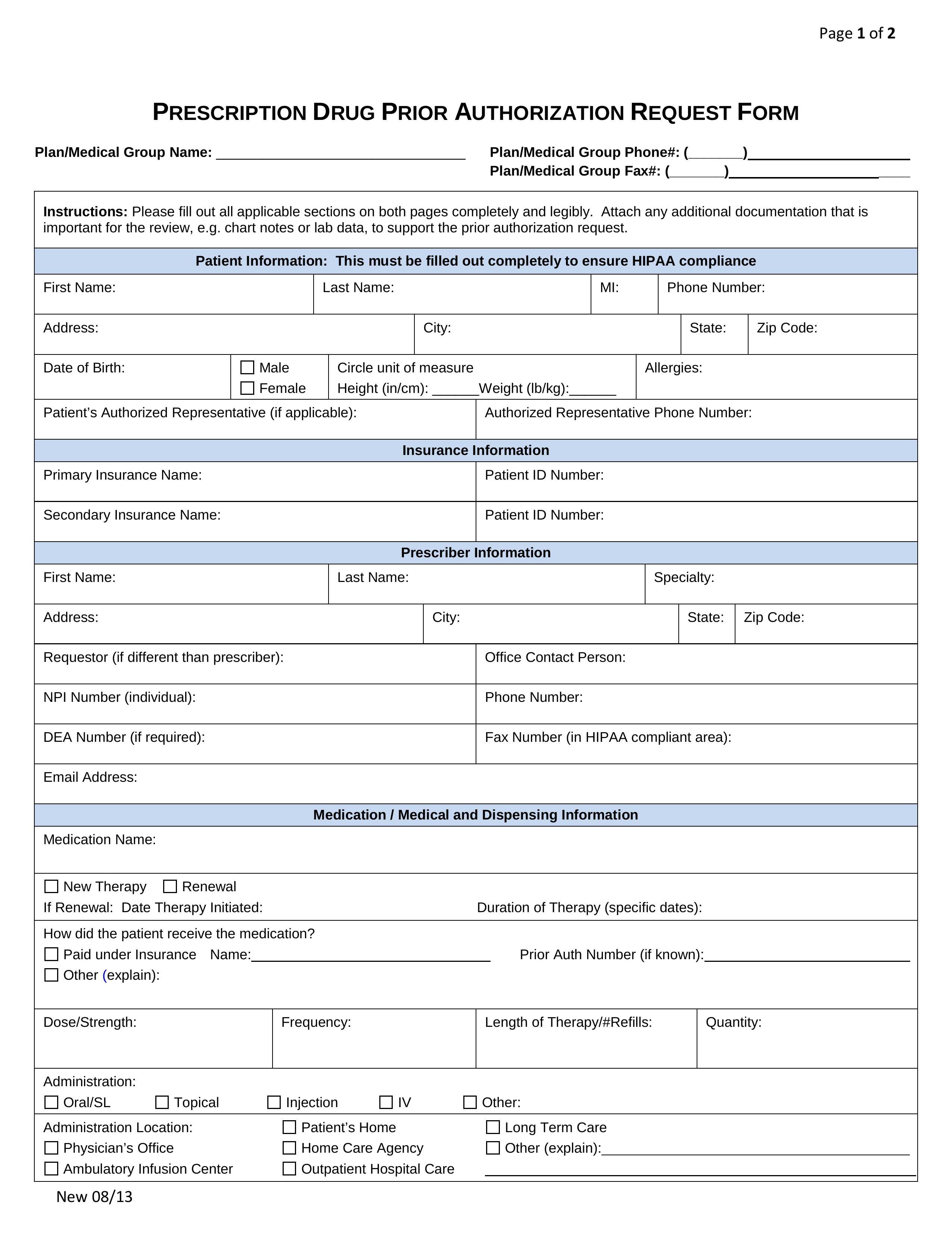
Fill out and submit this form to request prior authorization pa for your medicare prescriptions. Emergencies do not require prior authorization an emergency is a medical condition manifesting itself by. Prior authorization pa cross reference updated 81120.
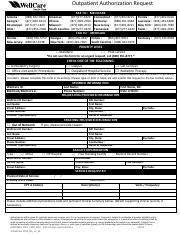
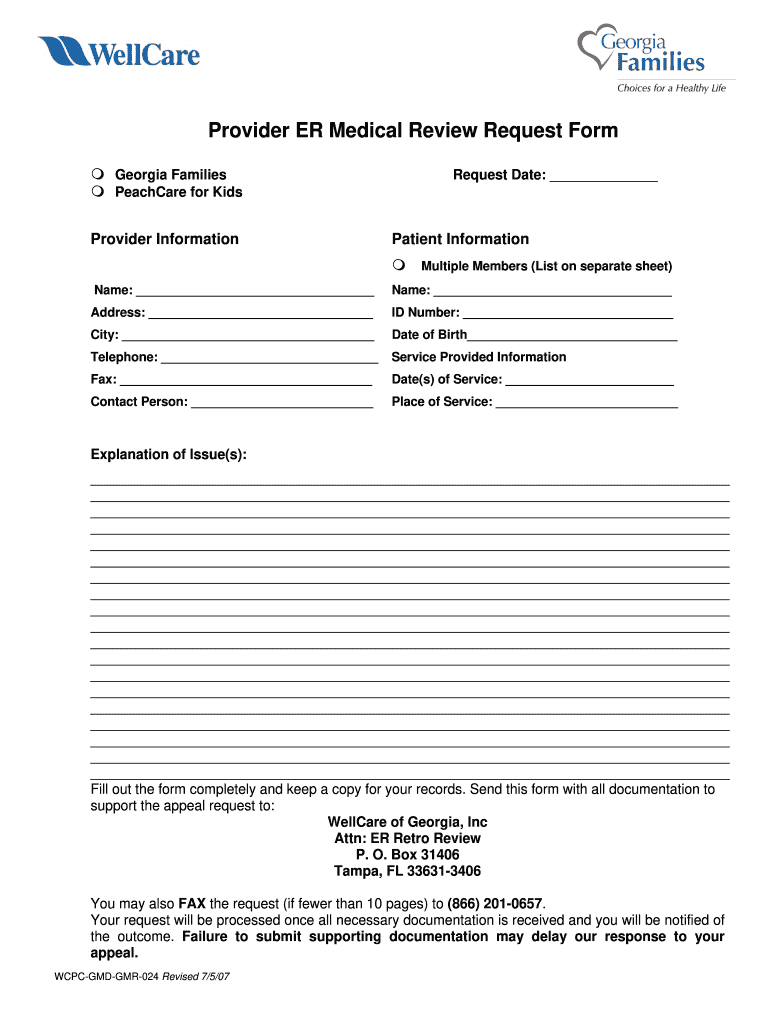
Cwellcare 2014na0714 fax to. A wellcare prior authorization form is a document used for requesting certain prescription drugs or coverednon covered services. A repository of medicare forms and documents for wellcare providers covering topics such as authorizations claims and behavioral health.
Forms for authorization behavioral health pharmacy services and miscellaneous purposes for wellcare of georgia providers. Failure to do so may result in denial of. But it substantially provides current authorization requirements.
This form is used to determine coverage for prior authorizations non formulary medications see formulary listings at. Prior authorization requirements are subject to periodic changes. Wellcare may grant multiple visits under one authorization when a plan of care shows medical necessity for this request.
061876 pro na caid 2014 outpatient authorization request form author. Authorization does not guarantee payment. It is usually necessary that previous therapies have been tried and failed in order for insurance companies to justify the prescribing of a more expensive.
The wellcare prescription drug coverage determination form can be used for prior authorization requests the demand by a healthcare practitioner that their patient receive coverage for a medication that they deem necessary to their recovery. Wellcare will evaluate the request based on applicable medical criteria fda.